In Focus
May 15, 2024
- Veterinary Science
Man’s best friend can also benefit, as canine iPS cells create world of possibilities
Professor Shingo Hatoya
Department of Veterinary Science, Graduate School of Veterinary Science
Osaka City University alumni Professor Shinya Yamanaka of the Center for iPS Cell Research and Application at Kyoto University announced the world’s first successful generation of iPS cells in 2006, and for this achievement was awarded the 2012 Nobel Prize in Physiology or Medicine. Attracting worldwide attention as it expands the possibilities of regenerative medicine and drug discovery, iPS cell research is also advancing in the field of veterinary medicine.
Under the leadership of OMU Professor Shingo Hatoya, a research group involved in veterinary regenerative medicine announced in 2021 that they had succeeded in generating canine iPS cells from the blood cells of dogs. What impact will this achievement have on dogs, their owners, society, and our health? We asked Professor Hatoya for his insights.

With the hope of reducing the burden on the dog’s body, the challenge began
Among the stem cells that give rise to other cells, pluripotent stem cells can differentiate into almost all of the cells that make up the body. iPS cells are one type of pluripotent stem cell. They are called induced pluripotent stem (iPS) cells because they are cells that have already differentiated and then are modified to return to an undifferentiated state before being transformed into other types of cells.
“Stem cell-based therapies have become common in recent years, not only with humans, but also in veterinary medicine for dogs and cats,” explained Professor Hatoya. “Although there are ways of regulating the immune system by administering the body’s own stem cells, pluripotent stem cells are not used. Recently however, many veterinarians are researching the possibility of regenerative medicine that uses stem cells like iPS cells to treat diseases that until now have gone uncured.”
In fact, research on canine iPS cells has been underway for quite some time, and iPS cells have been successfully generated from fibroblasts of excised skin and other cells. Obtaining the original cells, however, has been a major hurdle.
“We had to anesthetize the dog and remove some skin, which adds an extra burden on the animal. It’s not good to cause pain for the sake of research,” insisted Professor Hatoya. “Also, there is diversity among dogs, and if we only generate iPS cells from a specific breed, this limits our research. Furthermore, even if we wanted to generate iPS cells from a dog with a certain genetic disease to elucidate its pathology, it would be too much of a burden on both the animal and the owner to anesthetize the sick dog and cut off its skin. If it was possible to generate iPS cells from blood cells, we could ask for a portion of the blood that would be used for testing, which is something the owners should be willing to allow. With this in mind, we began research on the generation of iPS cells from blood cells.”

After trial and error, we succeeded in returning blood cells to an undifferentiated state with a high probability of success
According to Professor Hatoya, although canine iPS cells have already been generated from fibroblasts, the success rate was still unsatisfactory. Within the veterinary community, it was also considered difficult to generate iPS cells from canine blood cells. How did Professor Hatoya take on such a difficult challenge?
“In order to create iPS cells, you must reprogram the cells, that is, return them from a differentiated state to an undifferentiated state. Nobel Prize laureate Professor Yamanaka showed that cells can be reprogrammed by introducing four genes called the Yamanaka factors. When we introduced these genes into canine fibroblasts, we were able to generate iPS cells, albeit inefficiently. When we introduced them into blood cells, however, it did not work at all. It took trial and error before we realized that introducing the Yamanaka factors alone was not enough.”
Veterinary medicine has a smaller population of researchers than human medicine, and depending on the topic of research, there might be no precedents for reference. The same was true for the generation of iPS cells from blood cells, which could only be attempted by referring to the research methods of humans and mice that came before.
“Even the medium for culturing cells, in other words, the growth environment for iPS cells, is different for humans and mice,” Professor Hatoya explained. “It took us a long time to realize that the environment for dogs is more similar to that of humans than mice, but even under the same conditions, it did not work.”
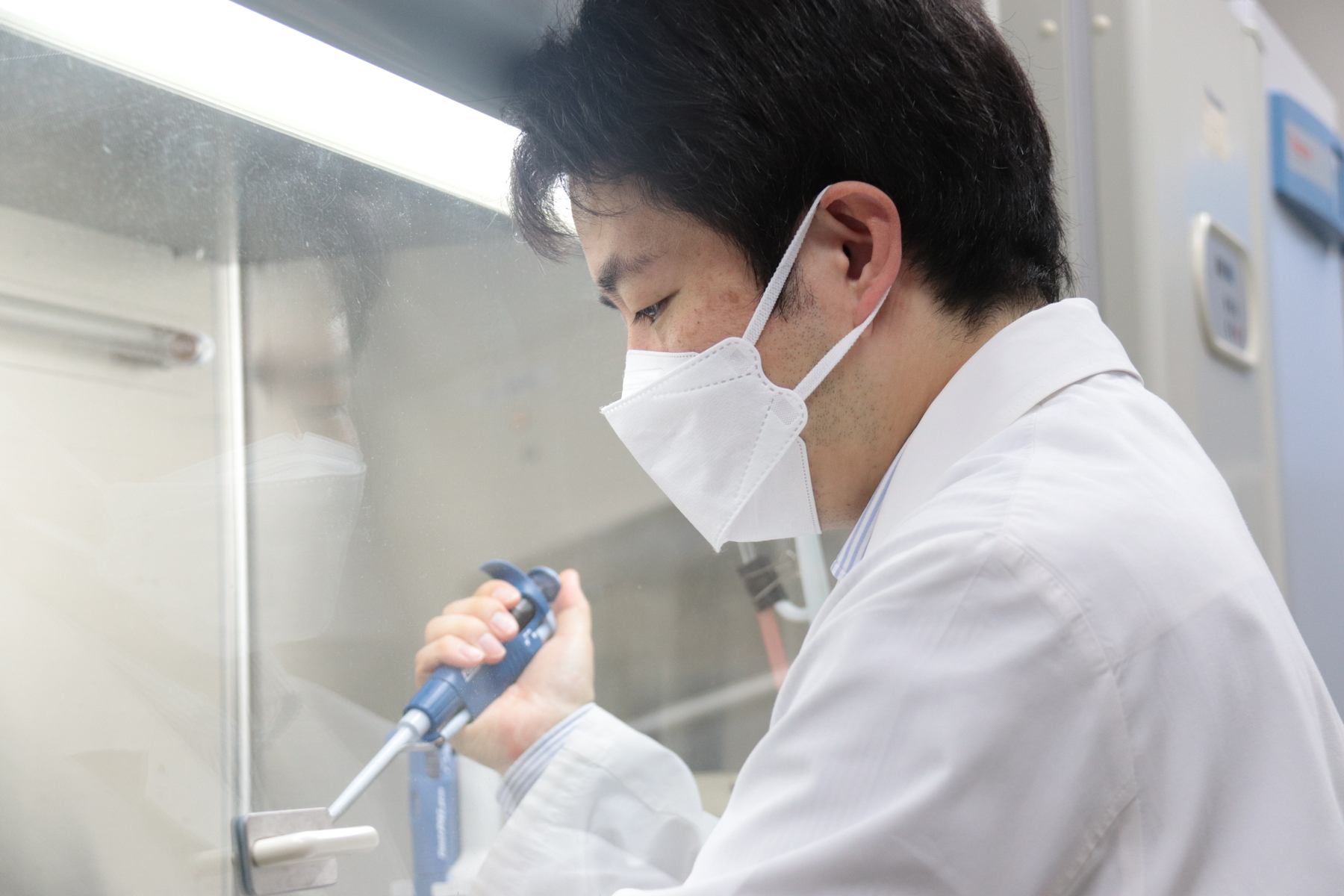
Despite taking more than 10 years to find success, students were always there to support the professor. Every year, students interested in doing clinical work and research on dogs and cats would enter Professor Hatoya’s laboratory, where, as an active veterinarian, he continued to see patients at the attached veterinary clinic. He looks back on how busy and difficult it was for him to continue working on both his medical examinations and his research.
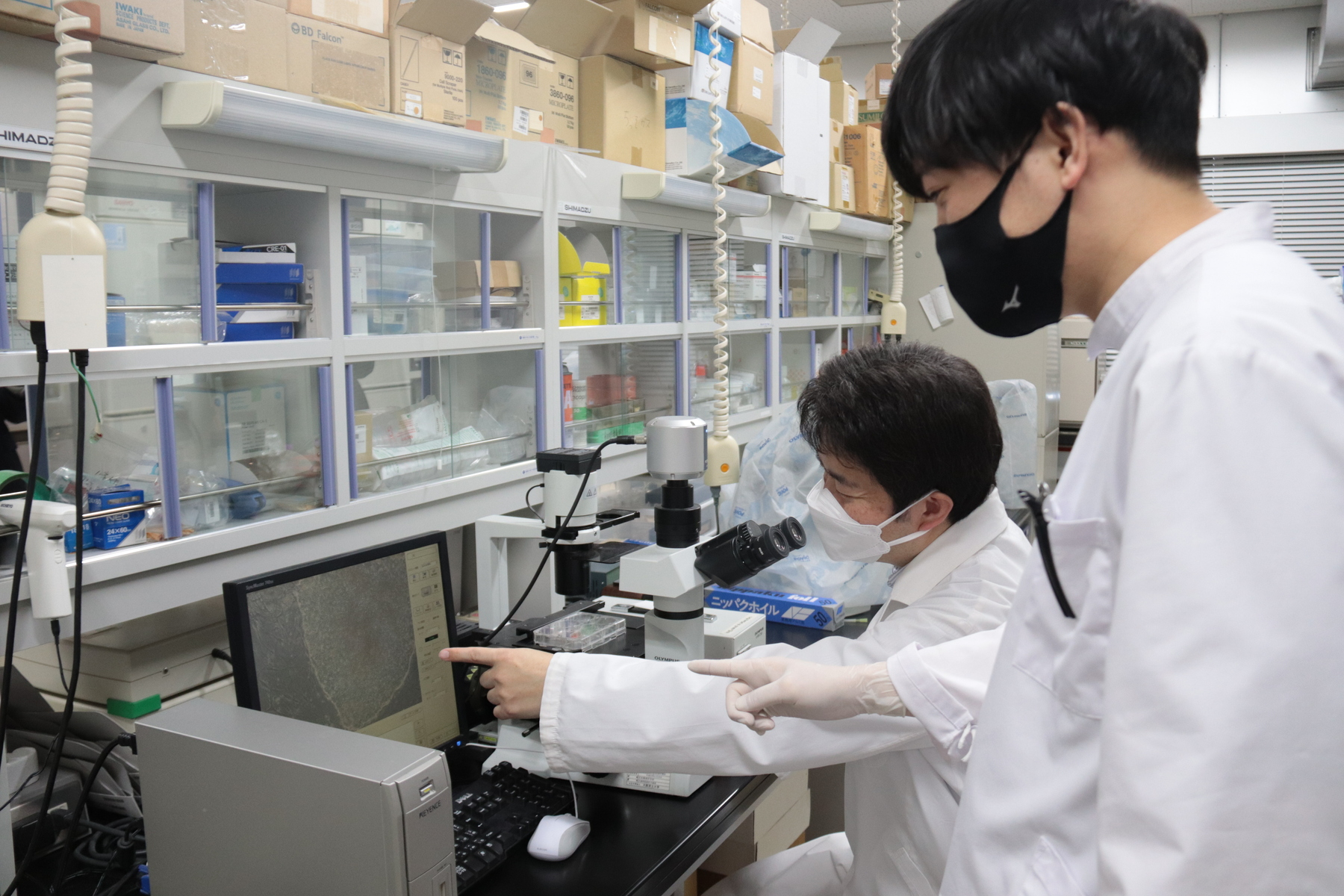
“I was able to maintain a high level of motivation because of the enthusiasm and hard work of the students. As time went by, research on human iPS cells progressed, and more and more information became available that could be used as a reference for canine iPS cells,” Professor Hatoya shared. “After trying various techniques, I found I could better promote reprogramming by adding and mixing several kinds of low molecular compounds in a certain state, allowing canine iPS cells to be generated with a higher probability. If I had proceeded alone, I would have given up halfway through. My research progressed thanks to the many professors who helped me and the strong passion of the students who worked by my side.”
Differentiation into various cell types can be used for regenerative medicine and blood transfusions
After much struggle, the generation of canine iPS cells from canine blood cells had finally seen success. With a process of generation that decreases the burden on the dog’s body, what should we expect to see in the future?
“First of all, this success will promote regenerative medicine in the veterinary field. We have received requests from domestic and overseas research institutions to provide them with canine iPS cells that we have generated, and after signing a contract with our university, they have begun to use the cells in their research,” extoled Professor Hatoya. “Next is research on the generation of blood for transfusion. It is said there is a shortage of human blood, but if so, there is an even greater shortage for dogs and cats. After all, they can't come in to donate blood on their own!”
We often hear that it is not rare to find dogs and cats in dire situations; a tumor surgery cannot continue because there is a lack of blood for a transfusion, for example. But if red blood cells could be generated from canine iPS cells, this situation would greatly improve.
“A graduate student at our laboratory recently gave a presentation at an academic conference about how we have succeeded in differentiating canine iPS cells to the preliminary stage of red blood cells. Once, we had to give up treatment for a large dog with leukemia. The dog was severely anemic due to a decrease in blood production. We treated him with anticancer drugs, but before the symptoms subsided, the anemia progressed, and we ran out of blood for transfusions,” lamented Professor Hatoya. “If I had more blood, I could have continued the treatment. The regret I felt at that time led me to research the possibility of generating red blood cells from iPS cells.”
The goal is to apply findings from clinical research in veterinary medicine to human health care
The advantage of using blood cells is that it is easy to generate canine iPS cells from various breeds and even from dogs that are patients, according to Professor Hatoya. As they can be easily generated from samples obtained from blood tests, it is possible to generate iPS cells from a large number of dogs, which will advance the understanding of pathological conditions and cell-level analysis of treatment methods.
“We believe that iPS cells can be used for genetic disease research and regenerative medicine, as well as contributing to various types of veterinary medicine, such as disease modeling and drug discovery. Although lab animal numbers are already decreasing considerably, our research will also help to reduce the number of animals used as laboratory specimens. I believe this is important not only for veterinary medicine, but for many other research fields that use laboratory animals.”
Now that he has achieved his goal of generating canine iPS cells from blood cells, where will Professor Hatoya look next for his research?
“I would like to find more stable conditions for culturing canine iPS cells and improve the efficiency and precision of the culture process,” he suggested.
“We are also, in parallel, conducting research on the generation of cat iPS cells, with the establishment of such research acting as a major theme. A large percentage of older cats suffer from chronic kidney disease. In recent years, research on the creation of mini organs called organoids using embryonic stem cells and iPS cells has been gaining momentum in humans. If this technology could be used to create small kidneys for cats, it should be possible to use it to shed light on why they suffer from diseases like chronic kidney failure. I would like to continue my research so that I can be of some help here,” Professor Hatoya proposed.
“In addition, a graduate student in our laboratory is conducting research on the possibility of generating sperm and eggs from cat iPS and embryonic stem cells and applying them to in vitro fertilization for the breeding of endangered species. While it is difficult to move individual animals, sperm and eggs can be transported easily, so worldwide fertilization should lead to the conservation of species while preserving genetic diversity.”
Professor Hatoya also hopes that his research will have a positive impact on human medicine. Could the advancement of iPS cell research in dogs and cats be useful for people?
“Dogs and cats live similar lives to humans, and as such, many of the chronic diseases they suffer are common to humans as well. My ultimate goal is to apply the knowledge I have gained from veterinary medicine to people. Currently, I am referring to the work of advanced researchers, but I hope to continue my own research and compare the similarities and differences between humans and animals.”
Professor Hatoya and his team’s research has produced significant results over an extended period of time. There are high expectations that their research will further contribute to the health of not only dogs, but other animals, including us.
Researcher’s details

Professor Shingo Hatoya
Professor, Department of Veterinary Science, Graduate School of Veterinary Science. After serving as assistant professor and associate professor in the Department of Veterinary Science, Graduate School of Life and Environmental Sciences, Osaka Prefecture University, he has been in his current position since 2022.
PhD (Veterinary Science).
Specializes in veterinary regenerative medicine. His main research interests include regenerative medicine using canine and feline iPS cells, establishment of feline in vitro fertilization methods and embryonic stem cell lines, and treatment of intractable medical diseases using mesenchymal stem cells. He succeeded in generating canine iPS cells from canine blood cells, publishing the results in the journal Stem Cells and Development in January 2021. He also succeeded in generating iPS cells from canine urine-derived cells, and the results were published in Stem Cell Reports in December 2023.
SDGs
